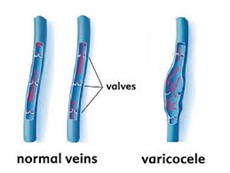
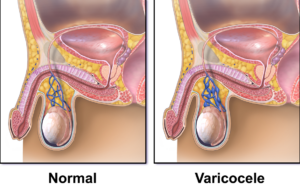
Sometimes, one or more of the veins of the spermatic cord may become enlarged and develop an abnormality known as a varicocele.
These veins are known as the pampiniform plexus. A varicocele only develops in the spermatic cord, and nowhere else. It is similar to varicose veins found in the legs. It can cause several issues and may contribute to male factor infertility.
What is a Varicocele?
Male infertility caused by a varicose vein of the testicle and scrotum – called varicoceles – is a very common occurrence, affecting approximately 10 percent of all men.
The varicose vein – very similar to those located on legs – happens when the vein valve fails and blood pools, enlarging the veins around the testicle and causing a varicocele. When this condition occurs, not only does it cause infertility, but it may also cause pain and testicular atrophy.