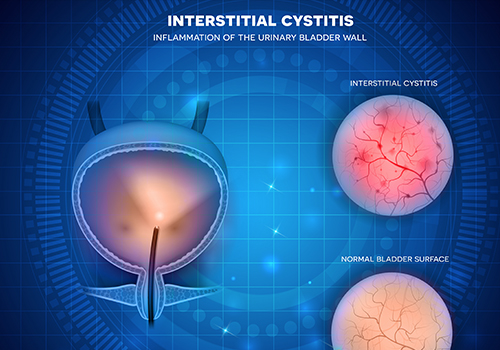
Interstitial cystitis (IC) or Painful bladder syndrome (PBS) is pain, pressure or burning in the bladder area and/or urethra accompanied by frequency or urgency of urination.
The symptoms last greater than 6 weeks and are not caused by other factors like bacterial infection, bladder stone or kidney stone. The symptoms may mimic a urinary tract infection as the condition is caused by inflammation or sensitivity of the bladder lining. Other common symptoms are pelvic pain, pain with intercourse and hematuria. Typically, pain increases as the bladder fills and decreases temporarily after urination. IC/PBS affects both men and women but is most common in females between the ages of 30 and 60 years old. The symptoms can greatly impact quality of life.
 Although research has not shown any definitive cause for IC/PBS there are several conditions that are frequently associated including:
Although research has not shown any definitive cause for IC/PBS there are several conditions that are frequently associated including: Diagnosis of IC/PBS is a diagnosis of exclusion. Your provider will conduct a history and physical exam initially to rule out other conditions that could cause the symptoms of IC/PBS. This may include a pelvic examination. Your urine will be checked in the office for signs of infection and blood. You may be asked to complete a symptom score sheet to help make the diagnosis and track the progress of your symptoms. Depending on your symptoms and other variables a cystoscopy (look in the bladder with a camera) and/or bladder pressure testing may be recommended.
Diagnosis of IC/PBS is a diagnosis of exclusion. Your provider will conduct a history and physical exam initially to rule out other conditions that could cause the symptoms of IC/PBS. This may include a pelvic examination. Your urine will be checked in the office for signs of infection and blood. You may be asked to complete a symptom score sheet to help make the diagnosis and track the progress of your symptoms. Depending on your symptoms and other variables a cystoscopy (look in the bladder with a camera) and/or bladder pressure testing may be recommended.
