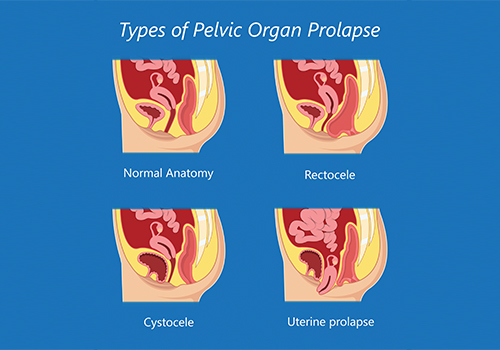
Pelvic organ prolapse (POP) is when one or more pelvic organs drops from the normal position causing a vaginal bulge.
These pelvic organs include bladder, uterus, small bowel and rectum. Prolapse can cause pelvic pain, pressure, difficulty urinating or defecating, frequency and urgency of urination and pain with intercourse.
 Pelvic organ prolapse is caused by weakening or injury to the pelvic floor muscles. These muscles act like a hammock to keep the pelvic organs in place. Pregnancy and childbirth are the main causes of POP but it can also be seen with normal aging, menopause and obesity.
Pelvic organ prolapse is caused by weakening or injury to the pelvic floor muscles. These muscles act like a hammock to keep the pelvic organs in place. Pregnancy and childbirth are the main causes of POP but it can also be seen with normal aging, menopause and obesity.
