Active Surveillance
Active Surveillance is an appropriate way to manage low risk prostate cancers in carefully selected patients. Nearly 30% of prostate cancers are slow growing. Active surveillance involves monitoring these cancers that have a low risk of progression to deadly disease. Most active surveillance protocols involve periodic PSA checks, annual DREs, and rebiopsy or reimaging within 12-18 months from diagnosis as long as the PSA remains relatively stable. The rationale to employ active surveillance is to avoid / delay treatment-related side effects from treatment with surgery or radiation as long as it is unlikely to demonstrably increase risk of a poor outcome from prostate cancer. Active surveillance is not appropriate for all prostate cancers and requires diligent follow-up and communication with your urologist. Active surveillance is often a “bridge to treatment”.
External Beam Radiation
External beam radiation is one of the standard treatments for prostate cancer and has similar outcomes to surgery in appropriately selected patients. It involves administration of ionizing radiation targeted at the cancer cells to damage the DNA so the cancer dies. The radiation is delivered by a radiation oncologist who administer the radiation with the aid of imaging. Typical treatments can last up to 8 weeks, but shorter “hypofractionated” regimens can be used in certain patients as well and can be as short as 5 treatments. The radiation oncologist will help determine what treatment regimens are most effective for you and your particular cancer.
Brachytherapy
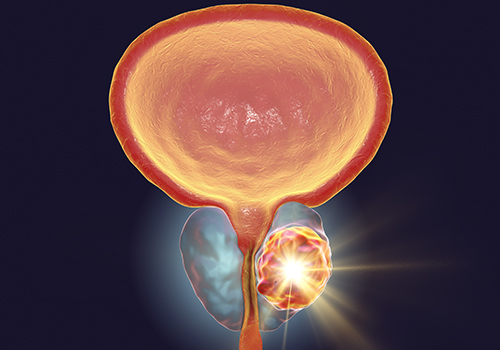
Brachytherapy is appropriate for men requiring treatment for low and favorable intermediate risk prostate cancer. This involves placement of radiative seeds into the prostate during a single surgical procedure by the urologist, who places the seeds with needles through the perineum, and the radiation oncologist who “doses” the radiation, and helps determine the optimal seed placement to maximize the damage to the cancer and minimize the damage to the normal surrounding tissues.Possible side effects of radiation treatments for prostate cancer include erectile dysfunction, damage to the bladder or rectum, urethral strictures, and rarely secondary cancers, such as bladder cancer.
Surgery
In the last 15 years robotic surgery for prostate cancer has become the standard surgical treatment for prostate cancer. Robotic-assisted laparoscopic radical prostatectomy first involves making 6 small incisions across the abdomen. The surgical robot arms are them placed within the abdomen after insufflation of the abdomen with CO2 gas. The robotic interface allows the surgeon to surgically reconstruct the bladder to the urethra after the prostate is completely removed. The surgeon controls every movement of the robotic arms and the camera. Several studies show a shorter recovery period and less blood loss with robotic prostatectomy as compared with the older “open” surgery. Despite the “minimally invasive” approach to robotic prostatectomy, it is a major surgery and typically involves a single night in the hospital and a urethral catheter stays in place for 7-14 days to allow healing. In the initial weeks to months after surgery, it is expected and common to have incontinence or leakage of urine, and patients will need to wear adult diapers and/or pads. Incontinence improves over the first year following surgery. Physical therapy, including Kegel exercises, can build up pelvic floor muscles and help some patients who are having persistent incontinence. If incontinence persists, which is rare, additional surgeries can be offered to improve urinary control. Another possible side effect from surgery is erectile dysfunction. This typically improves after surgery but in some cases can sometimes be permanent. Many treatments are available to help men who experience ED after surgery. Below is a link to Intuitive Surgical, makers of the Da Vinci surgical robot, which we use to perform radical prostatectomy at AAUrology.
 The prostate is a gland of the male reproductive system. It is located just below the bladder and comprises part of the male urethra. The prostate produces some of the fluid in semen and is involved in fertility. The seminal fluid protects sperm as they travel toward an egg. The prostate gland is active during ejaculation at which time sperm is ejected from the testes to the prostate. The seminal fluid is propelled into the urethra by the muscles of the prostate gland and the seminal vesicles.
The prostate is a gland of the male reproductive system. It is located just below the bladder and comprises part of the male urethra. The prostate produces some of the fluid in semen and is involved in fertility. The seminal fluid protects sperm as they travel toward an egg. The prostate gland is active during ejaculation at which time sperm is ejected from the testes to the prostate. The seminal fluid is propelled into the urethra by the muscles of the prostate gland and the seminal vesicles. The American Urological Association recommends prostate cancer screening begin at Age 55 for men of average risk and continue until age 70. They recommend screening start earlier for men in high risk categories (African American or with a positive family history). The AUA does not recommend routine screening in men over the age of 70 or in those with a life expectancy <10 years. We at AAUrology recommend any man consider prostate cancer screening with DRE and PSA who is concerned about death from prostate cancer. There are no side effects from prostate cancer screening. We strongly encourage African American men and with a family history of prostate cancer begin screening early at around age 40. The earlier prostate cancer is detected, the more options are available for treatment, and the better chance at cure.
The American Urological Association recommends prostate cancer screening begin at Age 55 for men of average risk and continue until age 70. They recommend screening start earlier for men in high risk categories (African American or with a positive family history). The AUA does not recommend routine screening in men over the age of 70 or in those with a life expectancy <10 years. We at AAUrology recommend any man consider prostate cancer screening with DRE and PSA who is concerned about death from prostate cancer. There are no side effects from prostate cancer screening. We strongly encourage African American men and with a family history of prostate cancer begin screening early at around age 40. The earlier prostate cancer is detected, the more options are available for treatment, and the better chance at cure.
